FOR IMMEDIATE RELEASE | August 17, 2008
Chemists move closer toward developing safer, fully-synthetic form of heparin
PHILADELPHIA, Aug. 17, 2008 — Chemists are reporting a major advance toward developing a safer, fully-synthetic version of heparin, the widely used blood thinner now produced from pig intestines. The U. S. Food and Drug Administration last spring linked contaminated batches of the animal-based product, imported from China, to more than 80 deaths and hundreds of allergic reactions among patients exposed to the drug for kidney dialysis and other conditions.
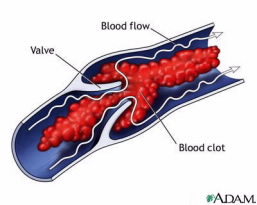
Described here today at the ACS’s 236th National Meeting, the purer, non-animal version could improve the drug’s safety and bolster regulatory control of its manufacture, the researchers say. Scientists expect demand for heparin, which prevents blood clots, to increase in the future due to rising rates of diabetes, heart disease, and other health complications linked to sedentary lifestyles. Global heparin sales total about $4 billion annually.
Contact
215-418-2407 (Philadelphia, Aug. 17-21)
202-872-4400 (Washington D.C.)
“With the problems associated with contaminated heparin produced from pig tissues in China, a non-animal source of this essential drug is gaining importance,” says study co-author Robert J. Linhardt, Ph.D., a chemist with Rensselaer Polytechnic Institute in Troy, New York. “A safer version of the drug could result in less adverse effects and fewer deaths.”
Heparin can be given by injection to prevent life-threatening blood clots during heart surgery and kidney dialysis. It also is used to clean intravenous lines used in those procedures. Because heparin is difficult to make in the lab from scratch, the drug’s only source has been from pig intestines.
Linhardt points out that processing of pig intestines to extract the raw materials is often done in small, family-run workshops in China, which supplies about 70 percent of the world’s heparin. Those mom-and-pop shops often fall outside the normal supervision and regulatory control standard in the pharmaceutical industry. The lack of oversight increases the risks of heparin contamination or adulteration with harmful chemicals, viruses, or other agents, he says.
“If heparin is prepared the right way, it should be consistent and safe, even from an animal source,” says Linhardt, who was part of the team that identified the suspected chemical contaminant in the Chinese heparin. The contaminant, called oversulfated chondroitin sulfate, can cause life-threatening allergic reactions. Heparin supplies containing the contaminant have now been recalled.
Researchers have been trying for years to develop heparin production methods that don’t require pig intestines. The first so-called total synthesis of heparin, developed in 2003 at the Massachusetts Institute of Technology (MIT), was not practical. It produced only minute batches of heparin — less than 0.000000035 ounces at a time — and could not be scaled up for commercial use, Linhardt says.
Working with Jian Liu, Ph.D., a medicinal chemist with the University of North Carolina-Chapel Hill, and Jonathan Dordick, Ph.D., a Rensselaer chemical engineer, Linhardt’s team now has developed an alternative synthesis method that boosts heparin production a million times higher than the MIT technique. The scientists employed a patented biotechnology approach that uses powerful enzymes to string together the individual carbohydrate units that form the pure heparin polymer. “Our biotech version of heparin will be prepared in a controlled environment ensuring that it is pure and free of contaminants,” Linhardt says.
So far, only small amounts of the new heparin have been produced in the laboratory using this technique, called “chemoenzymatic synthesis.” But Linhardt reports that the new approach can be used to produce the drug on a larger scale suitable for industrial manufacture. Cost, dosing, and administration of the new drug should be the same as conventional, animal-based heparin, he notes.
Linhardt plans to begin testing the synthetic heparin on animals this summer. If these and other tests are successful, the new heparin could reach the consumer market in two to five years, he estimates. The National Institutes of Health provided primary funding for the project.
# # #
— Mark T. Sampson
Robert J. Linhardt, Ph.D., is a professor in the departments of Chemistry, Chemical & Biological Engineering, Biology at Rensselaer Polytechnic Institute in Troy, New York. He is also Acting Director of RPI’s Center for Biotechnology and Interdisciplinary Studies.